Archive page
Migraine Neck Pain
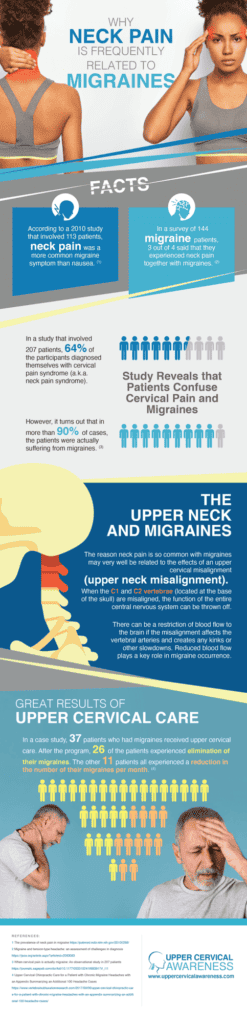
Neck pain may actually be the most common migraine symptom despite the fact that it is rarely listed among usual symptoms such as nausea and light sensitivity. According to one study in 2010 that involved 113 patients, neck pain was even more common than nausea. In a survey of 144 migraine patients, 3 out of 4 said that they experienced neck pain together with migraines. 60% of those who experienced neck pain said that it started before a migraine, making it a precursor to migraines and about three times more common than migraines with aura.
If neck pain is one of the most common symptoms of migraines, both before and during an attack, it is clear that the two are linked. So why is this an often-overlooked symptom? What is the connection between the neck and the head? We’re about to take a comprehensive look at the structures of the neck and why misalignments in the neck may lead to migraines.
Let’s begin by discussing some telling research in Italy that clearly connects neck pain and migraines.
Study Reveals that Patients Confuse Cervical Pain and Migraines
The research involved a study of 207 patients. 64% of the patients diagnosed themselves with cervical pain syndrome (a.k.a. neck pain syndrome). However, it turns out that in more than 90% of cases the patient was actually suffering from migraines. This makes a good case for seeing an expert in the neck for evaluation.
Some of the reasons that patients believed they suffered from cervical pain syndrome included:
- The pain started in the back of the neck
- Weather changes triggered pain
- Patients experienced nausea and vomiting
- Other symptoms like dizziness and vertigo occurred
- Neck pain preceded other symptoms
- The condition ran in the family
All 6 of these symptoms accurately describe migraines. Unfortunately, as noted above, many do not realize that one of the most common migraine symptoms is neck pain that precedes or occurs along with the rest of the symptoms.
The 3 Roles of the Upper Cervical Spine (upper neck)
To begin, we need to explain the three primary functions performed by the upper cervical spine. Understanding these structures and their function will result in a better understanding of why neck problems can lead to migraines. These three primary functions are:
Protecting the brainstem and spinal cord.
The bottom of the brainstem extends into the C1 vertebrae and connects to the spinal cord at this vital juncture. The upper cervical bones (upper neck bones) are protection against damage to the brainstem and spinal cord. Thus, the C1 and C2 play a vital role in brainstem function and communication throughout the body. Even a slight misalignment can take these bones from being protectors to being part of the problem.
Supporting the head and facilitating movement.
The average head weighs between 10 and 14 pounds. This atlas (C1) balances the weight of the head. If the C1 becomes misaligned, the weight of the head can become distributed improperly. This puts excess pressure on the neck and throughout the back, resulting in pain, tingling and numbness, and other nerve and soft tissue issues. The C1 and C2 also facilitate more than half of the range of movement of the head due to their unique design that is different from any other vertebrae. Unfortunately, this wide range of motion also results in more common misalignments in these two bones.
Enabling blood flow to the brain.
The cervical vertebrae (neck vertebrae) contain openings called vertebral foramen. These passageways provide a place for the vertebral arteries that provide the brain’s blood and oxygen supply. These openings also make the cervical vertebrae unique. As a result, proper alignment of the cervical spine (neck) plays a key role in the brain getting the blood and oxygen it needs to function properly.
Knowing these points about the function and design of the cervical vertebrae is an important factor in understanding the connection between the spine and migraines.
The Upper Neck and Migraines
The reason neck pain is so common with migraines may very well be related to the effects of an upper cervical misalignment (upper neck misalignment). When the C1 and C2 vertebrae (located at the base of the skull) are misaligned, the function of the entire central nervous system can be thrown off because of the roles we just discussed that are carried out by these bones.
There can be a restriction of blood flow to the brain if the misalignment affects the vertebral arteries and creates any kinks or other slowdowns. Reduced blood flow plays a key role in migraine occurrence. The misaligned bones could potentially put pressure on the brainstem or spinal cord, and this pressure can cause malfunctions in communication between the brain and body. Brainstem function also has some link to migraines. But these are not the only issues that can lead to migraines.
Upright MRI Evidence
Additionally, the position of these bones can result in pooling of cerebrospinal fluid if proper drainage becomes inhibited. Research has been performed using upright MRIs to see the effect misalignments have on drainage. Some of these studies also show that upper cervical realignment can help to restore proper drainage and eliminate the effects.
These misalignments can also damage nerves and soft tissue, thereby causing pain and stiffness. Even for patients who do not have migraines, the tissue damage often causes pain first. However, it is important to note that upper cervical misalignments don’t always cause neck pain, so if you have migraines but don’t have neck pain, do not automatically assume that your upper cervical spine is in alignment. Doctors must examine your neck using specialized techniques and diagnostic imaging to be certain.
How Do Upper Cervical Misalignments Occur?
It is important to appreciate that you do not have to have sustained a serious neck injury to be dealing with an upper cervical misalignment. Any kind of head or neck trauma can cause this issue.
For example, if you have suffered a concussion while playing sports or a whiplash injury from a car accident, a misalignment is likely. But did you know that it takes a collision of only 5 mph to cause a whiplash-type injury? Thus, more than just a sports collision or a fender bender but even a simple slip and fall can result in the problems we are discussing here. Thus, many fail to mention their injuries when filling out a patient history.
So please keep this in mind when speaking to health practitioners about migraines. Even a desk job where improper posture is sustained throughout the day or a habit of looking down to check a mobile device over and over again can lead to a misalignment in the upper neck.
Extensive Research Involving Migraine, Neck Pain, and Upper Cervical Care
To back up this connection between migraines and neck pain, research was conducted involving migraines and upper cervical care. Upper Cervical Care is a subspecialty of chiropractic that focuses on gentle and precise adjustments of the C1 and C2 vertebrae. There is no twisting, cracking, popping or jerking of the neck involved with this specialty.
The research involved 11 patients who had never received care from an upper cervical chiropractor. Each patient had experienced between 10 and 26 migraine days for at least four consecutive months prior to the study. The patients also needed to report a minimum of 8 headaches per month that hit a 4 or higher on a pain scale of 0-10 in order to qualify. In this particular study, patients received NUCCA (National Upper Cervical Chiropractic Association) method of upper cervical care to correct misalignments.
What were the results of the study?
The average number of days with migraines being experienced by patients at the start of the study was 14.5 per month. After just one month of care, that average was reduced to 11.4 days per month. After two months of care, that number was further reduced to 8.7, nearly half of the headache days at the beginning of the research. The study only lasted two months, but it can be inferred that further care would lead to continued benefits.
Other factors in the study included the use of a MIDAS score. This number records the degree of disability resulting from a condition with a higher number indicating greater disability. In this study, the average degree of disability was decreased from 46.7 down to just 14.6 after two months of adjustments and observation.
The study also considered the quality of life of the patients in three areas: emotional, physical, and restrictive (ability to perform normal activities). With these figures, a higher number indicates a better quality of life. For patients, the following improvements occurred:
- Physical quality of life averages increased from 54.1 to 86.6
- Emotional quality of life averages increased from 53.3 to 81.2
- Restrictive quality of life increased from 38.4 to 73.5
You may be impressed to know that these patients received between one and five adjustments only as-needed.
Case Studies Involving Upper Cervical Care for Migraines, Neck Pain, and Headaches
Besides this study, there are many case studies involving both migraine and headache patients who have benefited from various forms of upper cervical care. In one compilation of 101 case studies, 37 of the patients were experiencing migraines (note that a different method of upper cervical care was used in these studies). All but 8 of those 37 patients could remember a head or neck trauma that preceded the onset of migraines.
What were the results of these 37 case studies? 26 of the patients experienced the elimination of their migraines, including two men and a woman who had daily migraines. The other 11 patients all experienced a reduction in the number of migraines per month. Several daily migraine sufferers were down to just one or two per month. Some patients received benefits in as little as 1 month of care.
The youngest patient was age 9. He had been experiencing 10 migraines per month following an injury. His condition completely resolved in just one month of care. The oldest patient was 67, and she experienced a reduction of her migraine days to just one per month.
How Upper Cervical Care Differs from General Chiropractic
The results of the studies noted above are very convincing when it comes to the benefits of upper cervical care for migraine patients. However, you may still wonder if upper cervical is right for you or whether you can get the same benefits from seeing just any chiropractor. Here is a little information on what makes upper cervical care unique.
Upper cervical is a unique subset of the chiropractic field. As noted in the studies above, there are several different methods when it comes to how practitioners determine the degree of the misalignment or the way the adjustment is administered to the upper neck. However, there are commonalities between each method, and the primary differences are between upper cervical and general chiropractic. Here are the main things that set upper cervical apart:
Gentle adjustments
No popping, cracking, twisting, or forcing of the spine. Doctors perform adjustments with low force corrections using either hands-on manipulation or an adjusting instrument.
As-need adjustments
After the moving back of the atlas and axis (C1 and C2) into their original position, future adjustments are less and on as-needed basis. If your examination reveals that your adjustment is holding, you won’t receive an adjustment, and you may be able to extend the time between visits. This provides a cost-effective approach to care.
Family-friendly care
Your great grandmother or your infant may not be able to handle the heavy-handed adjustments of general chiropractic, but upper cervical care is for everyone. This allows families to extend a holistic (whole body) approach to health care to each member of the family.
Frequently Asked Questions About Neck Pain Migraine
What helps a migraine neck pain?
Ice pack helps to ease migraine neck pain. The cold therapy decreases blood flow and reduces inflammation thus relieving the pain. You can also place a cold pack on the forehead, temple, or neck.
Can tight neck muscles cause migraines?
Answer is yes, it can. People who have cervicogenic headaches experience a headache accompanied by neck pain. There are neck movements that can trigger such headaches.
How should I sleep with neck pain?
Two of the best sleeping positions when suffering from neck pain are on your side or on your back. Choose a rounded pillow to support the natural curve of your neck, with a flatter pillow cushioning your head when sleeping on your back.
Start Feeling Better Today!
Schedule a complimentary consultation to see how Sound Corrections can help you.
Schedule an AppointmentContact UsHeadache and Migraine Triggers
Chronic and recurring headaches can suck the joy out of your life and negatively impact everyone around you. It can cause you to miss out on family vacations, gatherings, client proposals, school projects, and other kinds of events that matter to you. To make things worse, finding a sustainable source of headache or migraine relief in Orem can come with a few hiccups if you have pre-existing health conditions or additional risk factors such as migraines, family history, and alcohol intake. Let’s take a closer look at the usual headache and migraine triggers below.
1. Migraine
Migraine is a complex neurological disease that triggers throbbing headaches, nausea, tunnel vision, and other symptoms. Patients who experience migraine-related headaches describe their pain as pulsing or pounding and limited on only one side of the head. Doctors and researchers categorize migraine under primary headache, denoting that it doesn’t stem from another medical condition. It can happen up to 15 or more each month, depending on a patient’s risk factors. Thousands of patients look for migraine relief in Orem to manage their episodes better and minimize the impact of the symptoms.
2. Genetics
According to research, headaches and migraines can be hereditary. So, if one or two of your family members experience frequent migraine attacks, you also have a high probability of having the same health problem.
3. Sinus Congestion
Headache is one of the most frequently reported symptoms of sinus congestion. When your sinuses swell due to an infection or allergic reaction, the pressure inside your head also increases, making you more susceptible to headaches.
To learn more about the connection between head and neck injuries and migraines and other headaches, download our complimentary e-book by clicking the image below.
4. Excessive Alcohol Consumption
Excessive alcohol intake can lead to serious health repercussions such as severe and more frequent headaches. Here are some of the usual adverse effects of drinking too much alcohol:
- Alcohol can impact your kidney – Binge drinking alcoholic beverages can lead to increased dehydration. It also affects our kidney function, making them less efficient in filtering wastes from your blood.
- Alcohol also can elevate your blood pressure – Unfortunately, when your blood pressure spikes, you can potentially develop a bad headache that can last for a few minutes to several hours.
- Alcohol affects serotonin release – Alcoholic beverages can increase the release of serotonin in the blood. That’s why many people who drink alcohol feel happier than usual. However, prolonged alcohol intake can lead to a drastic drop in serotonin levels, increasing one’s pain sensitivity and vulnerability to stress, frustration, and anxiety.
5. Strong Odors
Believe it or not, a strong odor plays a massive role in developing migraines and headaches. When you’re sensitive to strong scents and fragrances, you might experience nasal irritation, which can trigger allergy-like symptoms such as headaches and runny noses. Strong odors can also cause the blood vessels to swell. The swelling can stimulate the nerves associated with the onset of terrible headaches.
6. Unhealthy Sleep Patterns
Unhealthy sleep patterns cause the development of migraines and headaches in some people. If you don’t get enough sleep or sleep for too long, you may wake up with a heavy throbbing in your head. To prevent that from happening, you can do the following:
- Always aim for at least 8 hours of sleep every night.
- Sleep on your bed and not on the couch.
- Go to bed when your brain tells you that you’re sleepy and avoid distractions like TV or your mobile device.
- Avoid doing rigorous activities before heading to sleep.
- Keep your afternoon or morning naps short.
- Follow a consistent sleep schedule.
- Limit your caffeine consumption as it may interfere with your sleep pattern.
7. Emotional Stress
Headaches and migraines are more likely to occur when you are under a lot of stress. Studies have yet to fully explain the exact role of emotional stress in the onset of headaches. However, many people note worse attacks when they feel emotionally or mentally burnt out. Some researchers theorize that it might have something to do with the stress hormones, which can trigger inflammation, blood vessel constriction, and sudden surge of blood in various organs such as the brain.
8. Head and Neck Trauma
Head and neck injuries can potentially become the root cause of your headaches and migraines. According to case studies on natural migraine relief in Orem, many people who suffer from recurring migraine attacks have a history of neck and head trauma. Unfortunately, even after the damaged tissues heal, the spinal bones, like the C1 and C2, fail to back to their original position. This, in effect, impedes the normal flow of signals to the brain, triggering headaches and migraines attacks. Until the bones go back to their normal position, the symptoms will linger and cause severe impacts on your daily life.
Addressing the Underlying Causes of Migraines and Headaches
We hope that our discussion above helped you understand that headaches, especially chronic and recurring ones, rarely happen for no reason. If you notice increased severity or frequency of your headaches and previously sustained neck or head injury, we suggest scheduling your appointment with Dr. Beadle, our certified upper cervical chiropractic doctor. At Sound Corrections Chiropractic, we offer effective migraine relief in Orem. To do that, we assess the alignment of the C1 and C2 bones and determine how many adjustments or sessions you might need to restore your spine’s natural curvature. Once you start receiving the upper cervical chiropractic adjustments, you will notice changes in your symptoms and the severity of your migraines or headaches.
Start Feeling Better Today!
Schedule a complimentary consultation to see how Sound Corrections can benefit you.
Schedule an AppointmentContact UsMost of the time when migraine symptoms are topic in a discussion, they are listed in order by how common they are. What we are going to look at today are some of the most debilitating migraine symptoms. While the order is subjective, you will no doubt agree that migraines are more than just an ordinary headache. We also want to provide our readers with hope that migraines don’t have to lead to disability or lifelong medication use, so we will also discuss a way of finding natural relief from migraine symptoms.
The 6 Most Debilitating Migraine Symptoms
1. A Throbbing Headache
This is by far the most common migraine symptom, and it can be one of the most debilitating. The throbbing headache that affects most migraine patients can range from moderate to severe. Strain often increases the pain making strenuous physical activity difficult if not impossible during an attack. In about two-thirds of cases, the pain occurs on one side of the head, but that means about a third of migraine attacks affect both sides of the head. The throbbing or pulsing sensation is a telltale sign that a headache is actually a migraine symptom.
2. Sensory Sensitivity
This is the migraine symptom that sends most migraineurs heading to a dark, quiet room during an attack. Not only can bright lights, loud sounds, and strong scents trigger a migraine attack, but they can also make one that is in progress significantly worse. Even dim lights may seem exceedingly bright during a migraine attack, which is why sufferers seek dark rooms to recover. A normal sound, such as a loved one chewing, may suddenly seem to sound like a woodchipper being used. Even a normally pleasant scent, if it is too strong, could be overpowering during a migraine.
3. Neck Pain
The fact is that most migraineurs don’t complain about neck pain – until you place it on a list of symptoms in a questionnaire. Then you suddenly have 75% of responders admitting that neck pain usually occurs either before or during an attack. In fact, an Italian study found that many patients who thought they were suffering from cervical pain syndrome were actually dealing with migraines. Why did the confusion exist? A few reasons include:
Pain started in the back of the neck – Since most people associate migraines with headaches, pain starting in the neck caused patients to separate the symptoms.
Pain was triggered by weather changes – Most people associate weather and pain to mean arthritis. However, weather changes are among the most common migraine triggers.
Patients experienced dizziness or vertigo – While these symptoms are commonly associated with neck pain, they can also be migraine symptoms.
We’ll get into the link between neck pain and migraines again toward the end of our article.

4. Nausea and Vomiting
Nausea and vomiting can put a quick end to whatever you thought you were going to accomplish today. Combine this with sensory sensitivity, and you have the recipe for lying in bed in a dark room with a nearby bucket for emergencies. This is one of the most debilitating migraine symptoms. Fortunately, nausea is the more common of the two symptoms ,and most patients don’t actually reach the point of vomiting.
5. Dizziness or Vertigo
Whether you get a feeling of lightheadedness and faintness or the feeling like the room is spinning, you’re probably not going anywhere for a while. No one wants to be up and active when it feels like he or she may faint at any moment. And vertigo (a false sensation of movement), can often make nausea worse, especially a severe bout. A person may not even be able to shake the sensation of movement when lying down with his or her eyes closed.
6. Vision Changes
The vision can be affected in many ways by a migraine. We already discussed sensitivity to light, but other vision issues may include:
- Seeing flashing lights or zigzag lines
- Blurry vision
- Double vision
- Temporary loss of vision
- Pain behind one eye (this may affect your vision by forcing you to keep the eye closed)
Visual symptoms are present in migraines with aura or ocular migraines. While aura will likely affect both eyes and occur 20-30 minutes before a migraine, ocular migraines will affect just one eye and occur with or without a headache.
Since sight is an important part of most human activities, this can be a particularly debilitating symptom.
Dealing with Migraine Symptoms Naturally
If you experience migraines frequently, you may be searching for natural remedies for migraines. While there are some self-care practices you can perform at home (i.e., getting enough sleep, not skipping meals, keeping a migraine journal and avoiding triggers), we want to introduce you to a natural way to be proactive about your migraine care.
The neck is related to migraines in a number of ways. For example, the upper cervical spine protects the brainstem, but a misalignment can actually put pressure on the brainstem and inhibit proper function. The cervical spine facilitates blood flow to the brain, but a misaligned cervical spine can have the opposite effect. In fact, when the C1 is out of alignment, it may prevent proper cerebrospinal fluid drainage and lead to intracranial pressure.
It makes sense then why upper cervical chiropractic care, a subspecialty of chiropractic, is finding much success helping reduce the frequency and severity of migraines. In fact, some patients even find that complete resolution of their migraines after just one or two adjustments. To learn if you are a good candidate for this form of care, find a practitioner in your local area, and schedule a consultation.
Start Feeling Better Today!
Schedule a complimentary consultation to see how Sound Corrections can help you.
Schedule an AppointmentContact UsMigraine attacks happen to millions of people in the US. And yet, many people still have a lot of misconceptions about this highly prevalent symptom. From myths about going to a migraine chiropractor in Orem UT to migraines being just an ordinary headache, check out the list of 10 migraine myths you should stop believing in below.
10 Migraine Myths
1. Migraines and headaches are the same
Many people use headaches and migraines synonymously when they describe their pain to their doctor. Unfortunately, this only leads to confusion and failure to find a sustainable pain remedy. Take note that migraines attacks are a complex neurological problem that includes headaches and other symptoms like vomiting, nausea, fatigue, and sensory sensitivity.
2. Migraine attacks always occur with visual disturbances
Visual disturbances or aura like hazy vision, seeing wavy or flashing lights affect many migraineurs. However, it doesn’t mean that a migraine attack can’t happen without this specific symptom. According to the Migraine Trust Foundation, roughly 70 to 90 percent of migraine sufferers don’t experience aura. This type of migraine attack can last anywhere from four hours to a maximum of five days.
To learn more about the connection between head and neck injuries and migraines and other headaches, download our complimentary e-book by clicking the image below.
3. Migraines only affect women
Indeed, migraine episodes tend to occur more frequently in women than men. However, this doesn’t mean that only women suffer from this debilitating symptom. For the male population, migraine attacks have a prevalence rate of roughly 8.6 percent.
By age 10, most males tend to have a lower tendency of migraine episodes compared to females. This is primarily because of the estrogen level fluctuations in the females during the childbearing years. Estrogen level in the body is the main factor that influences the severity and frequency of menstrual and hormonal migraines in women.
4. Taking pain medication is the only option
Surely, pain medications like NSAIDs provide quick relief from common migraine symptoms like headaches. However, it’s crucial to note that you have plenty of other options if you want to experience lasting relief from your migraine attacks. For example, you can visit a migraine chiropractor in Orem UT, make lifestyle adjustments, avoid migraine triggers, and allocate enough time to exercise.
5. Changing your diet is key to experiencing ZERO migraine symptoms
Many people notice that their migraines tend to worsen when consuming certain food items, including those containing a high amount of salt and preservatives. As a result, some believe that changing their diet alone can eliminate their migraine symptoms once and for all.
In truth, migraine is a highly complex neurological problem, so a simple diet shift isn’t enough to see lasting results. You may need to include other lifestyle changes like skipping alcohol, improving sleep quality, and managing stress.
6. There’s only one type of migraine
Sadly, there are several types of migraines. They come with varying levels of intensity and severity. In most cases, patients who seek the help of a migraine chiropractor in Orem UT may suffer from migraines with or without aura. Knowing the key differences between these two and their sub-types can make a huge difference in managing your symptoms.
7. Caffeine triggers migraine attacks
Caffeine is a fascinating plant-derived substance as it has varying effects on migraineurs. Some claim that they experience worse bouts of headaches when they drink caffeinated beverages. Others, on one hand, explain that caffeine helps them cope. These varying accounts of migraineurs on caffeine might stem from the ingredient’s ability to reduce blood flow in the veins. If you drink excessively or consume lesser than usual caffeinated products, you might exacerbate your migraine symptoms.
8. Migraines only occur in high-stress individuals
Truth be told, migraine attacks can happen to anyone. Stress is just one of the many migraine factors that can trigger an attack. This is why even the calmest person can experience severe bouts of migraine headaches. It’s important to know what triggers your episode so you can make the necessary adjustments to your lifestyle.
9. Only adults and aging folks have migraines
Did you know that migraine episodes are among the main reasons for pediatrician clinic visits? That’s because about 10 percent of school-age kids experience migraine episodes. It’s also quite prevalent in teenagers and young adolescents. While the symptoms may not be as worse as those experienced by adults, dealing with migraines in kids can be equally challenging, especially when kids don’t know how to express what they experience.
10. Migraine attacks only happen once a month
The most unfortunate fact about migraine attacks is that they tend to occur several times each month. If you have the chronic type, you might have up to 15 episodes lasting anywhere from a few minutes to a couple of days. It’s crucial to seek a sustainable remedy option from professionals like a migraine chiropractor in Orem UT so that you can curb the impact of your symptoms on your usual routine.
Seeking Help From A Migraine Chiropractor in Orem, UT
Migraines attacks can be quite debilitating, especially if they frequently happen. Fortunately, you can potentially get rid of the symptom or attenuate their effects on your life with upper cervical care. This specific approach is quite helpful because it provides the following benefits:
- Improves communication between the brain and other parts of the body
- Restores the average flow of cerebrospinal fluid (CSF) and blood to and from your brain
- Eases stress and tension on nerves pressed by misaligned neck bones
Upper cervical care is a promising natural remedy for chronic migraines. If you have been experiencing worse symptoms, you might find it helpful to consult with an upper cervical chiropractor and have your neck bone alignment fixed.
Start Feeling Better Today!
Schedule a complimentary consultation to see how Sound Corrections can help you.
Schedule an AppointmentContact UsAs common as migraines are, silent migraines are relatively rare. Only about 3-5% of people will ever experience a silent migraine (which is still a lot more common than many other conditions), but the common migraine affects up to 12% of people. Silent migraines are difficult to diagnose, but that doesn’t make them any less serious or debilitating. Here are 7 things you should know about silent migraines. We’ll conclude by discussing a natural way that many are breaking away from the grip of migraines.
7 Silent Migraine Facts
1. Migraines Don’t Always Accompany a Headache
The difference between migraine and headache becomes clear when one realizes that there are several types of migraines that do not include any head pain. This is possible because migraines are more than just a bad headache. This is a neurological condition. For example, a person may experience a visual migraine or a migraine that begins with aura but doesn’t lead to a headache (called migraine dissocie).
2. Migraines Occur in Up to 4 Phases
The four phases of a migraine are:
- Prodrome – A warning phase that occurs up to 24 hours before a migraine actually begins
- Aura – Visual symptoms that usually occur 20-30 before a migraine
- Pain – The headache phase that many people use synonymously with the term migraine
- Postdrome – Up to 24 hours of symptoms that follow a migraine and are sometimes referred to as a migraine hangover
The only thing is, not every migraine includes all four phases and not every patient experiences all four phases. For example, only about 20-25% of migraineurs experience aura. Since about 85-90% of migraines include the pain phase, it throws some people off when this is the phase that is missing.
3. Silent Migraine Symptoms Can Still Be Debilitating
What are the symptoms of a silent migraine if there is no pain phase? One of the most common symptoms is aura, which is interesting because this is one of the less common phases among migraineurs in general. When a person experiences aura, he or she may see spots, wavy lines, flashing lights, or experience tunnel vision. Other effects can occur besides just the visual ones. Hearing problems (including auditory hallucinations), tinnitus, speech problems, vertigo, dizziness, and numbness and tingling may also be present.
Of course, aura is not the only symptom of silent migraines. The patient may also experience nausea and vomiting, diarrhea, irritability, fatigue, dizziness, and chills. When all is said and done, a migraine can be just as bad without the head pain.
4. Silent Migraines May Be Related to Blood Flow the Brain
While the direct cause of migraines has still not been determined, research points to a lack of blood reaching the cerebral cortex. As a result, many doctors classify migraines as neurovascular – resulting from a combination of changes in both the nervous and vascular systems. This is especially true if the patient is dealing with aura. We’ll discuss what can be disrupting blood flow to the brain a little later in our article.
5. Some Migraine Treatments Involve Off-Label Medication Use
Off-label use refers to a medication being prescribed for something other than what it was used for in clinical trials. Somehow doctors began to notice that some patients have fewer migraines on anti-seizure medications. It is important to remember, however, that these drugs have different effects on everyone. Some patients may experience fewer migraines while others may just get the side effects with no real benefits. The medications simply weren’t designed for this use, so the outcomes are uncertain.
6. Silent Migraines Have Similar Triggers as Migraines with Pain
Migraineurs know that everything from a sudden change in the weather to strong smells or bright lights can lead to the onset of a migraine with pain. The same is true for those who get silent migraines. Learning your migraine triggers can help you to avoid some of the circumstances that lead to migraines, but others are unavoidable.
7. Natural Relief for Migraines Is Available!
Remember that migraines, especially silent migraines or migraine with aura, seem to be related to blood flow to the brain. Well, proper blood flow to the brain is facilitated by the cervical spine. How? The vertebrae in the neck have tiny loops of bone called vertebral foramen. These allow a place for the vertebral arteries to flow through on their way to the brain.
Unfortunately, this means that a misalignment can affect that free flow of blood. It has been noted in numerous migraine and headache patients that an upper cervical subluxation exists. Correcting this misalignment has helped many people in case studies to experience fewer or less severe migraines. Some have even gone from dealing with chronic migraines (15 or more days per month with symptoms) to being completely migraine-free).

History of Head or Neck Injuries
It is no wonder that many migraine patients have a head or neck trauma somewhere in their patient history. If that sounds like you then you are probably a good candidate for upper cervical chiropractic care. This subspecialty of chiropractic focuses on the top two bones of the neck where the brainstem meets the spinal cord. These bones can affect both the nervous and vascular systems of the body when not in proper alignment. As a result, it just makes sense to get this area checked if you are experiencing migraines.
Upper cervical chiropractors are skilled in identifying even the slightest of misalignments in the C1 and C2 vertebrae using specialized diagnostic imaging techniques. To learn more, schedule a consultation with a practitioner near you.
Start Feeling Better Today!
Schedule a complimentary consultation to see how Sound Corrections can help you.
Schedule an AppointmentContact UsLet’s get one thing straight: a migraine isn’t just a terrible headache. In other words, a headache is different from a migraine. We’re here to help you tell them apart from one another.
Migraines are a neurological disorder that can affect the brain over time. Unlike a common headache, migraines involve other symptoms, not just a headache. In fact, a headache may be absent in a migraine. We’ve listed below the list of symptoms that can help you figure out if your headaches are actually migraines. Keep in mind that they aren’t all-inclusive, and only doctors can diagnose migraines.
Many people self-medicate to ease their migraines, unknowing that it can do more harm than good. Some over-the-counter pain relievers can make migraines even worse if not used appropriately. At the end of this blog, we will introduce a natural care that can help you get relief from both migraines and headaches.
List of Migraine Symptoms to Know
Watch out for these signs and symptoms that should clarify if your head pains are migraines.
Aura
Around 25% of people with migraines deal with aura 20-60 minutes before an extreme headache hits them. Aura comes in different forms like visual disturbances (seeing flashes of lights or zigzag lines, partial vision loss, blind spots, etc.) and sensory symptoms (tingling sensation in the face and arms, numbness, etc.)
Although aura is often the precursor to headache, it is not an indication that you will automatically have the head pain. Migraineurs who experience aura are more prone to depression and suicide.
Headaches
A headache falls into the category of a migraine if it meets at least two of these criteria:
- One-sided (Unilateral) pain
- Moderate to severe pain
- Pulsing or throbbing headache
- Pain that aggravates with exertion
It is a common headache if it only meets 2 of these 4 requirements. When dealing with migraines, you can have an extreme headache that intensifies with exertion, but it can also be just chronic achiness that affects both sides of your head.
Sensory sensitivities
Migraineurs frequently have sensory overload due to sensitivities. During an attack, they may find loud sounds, bright lights, and strong smells particularly overwhelming or painful. Not only that, they may perceive a gentle caress as an aching or burning sensation.
Nausea and vomiting
Nausea is another hallmark of migraines. Thankfully, vomiting is not as common. Only a few people experience it. According to the National Headache Foundation, migraine sufferers who experience nausea and vomiting during an episode might have a more severe kind of migraine that means worse attacks but fewer relief options.
Vestibular symptoms
Vestibular migraines account for 25-40% of all migraine cases. Migraines of this kind involve vestibular symptoms such as dizziness, tinnitus, and vertigo.
Neck pain
Migraineurs often overlook this symptom, but it is more common than they thought. In fact, a study showed as many as 75% of people with migraines experience neckache before or during an episode. This reestablishes the undeniable connection between migraines and the neck, which we will discuss thoroughly in the latter part of this blog.
As you can see, it’s not too difficult identifying migraines from a common headache. A headache does not involve most of these symptoms on the list. If you suspect you are dealing with migraines, here’s how you can get relief naturally. The very key is to address the often overlooked but underlying cause of many migraines.
Additional symptoms
As mentioned, many symptoms accompany migraines; some vary in frequency. Migraine patients may also experience a stuffy nose, making people mistake a sinus headache to a migraine. They may also deal with mood swings, eye pain, excessive yawning, food cravings, frequent urination, speech troubles, and many more. Frequent yawning is believed to be caused by the drop in blood flow to the brain.
Migraines Originate in the Neck
We should not ignore the fact that three-quarters of migraineurs experience neck pain. This truth holds the secret to natural relief to migraines. Neck pain can stem from a misalignment of the atlas vertebra in the neck (upper cervical spine). A misalignment, also called subluxation, can have far-reaching effects in the body. It may result in these:
- Restricted function of the brainstem
- Reduced blood flow to the brain
- Increased intracranial pressure caused by impaired cerebrospinal fluid drainage
These conditions can significantly contribute to the development and recurrence of migraines. Therefore, it makes perfect sense to repair an atlas misalignment to relieve and avoid migraines. With the help of upper cervical chiropractic, you can achieve it.
Receive Upper Cervical Chiropractic Care Today
Upper cervical chiropractors offer a unique form of care that is only practiced by more or less 3,5000 chiropractors worldwide. The technique involves exact measurements of the atlas misalignment and very gentle adjustments to fix the subluxation. Many of our patients enjoy the benefits they gain from this care alternative, such as fewer and less frequent migraine episodes and lasting relief.
Start Feeling Better Today!
Suffering from Headaches or Migraines? Contact us today!
Schedule an AppointmentContact Us